Our goal is to provide education and insight on healthcare topics related to Substance Use Disorder. To ensure we provide accurate and trustworthy information, our writers follow strict editorial guidelines.
Addiction is a complex and chronic disease that affects the brain and behavior, often leading to destructive outcomes. While many see addiction as simply the inability to stop using substances, the reality is far more intricate. The cycle of addiction involves brain chemistry, tolerance, withdrawal, and the body’s changing response to substances over time. Understanding these factors can help shed light on why breaking free from the cycle of addiction is so difficult and what happens biologically when someone becomes addicted.
The Role of Dopamine in the Addiction Cycle
At the heart of addiction or substance use disorder is dopamine, a neurotransmitter in the brain responsible for feelings of pleasure and reward. When someone uses drugs—whether opioids, stimulants, alcohol, or other substances—dopamine levels surge, creating a euphoric high. This “reward” encourages repeated use of the substance to relive those pleasurable sensations.
Over time, the brain begins to rely on the substance to produce dopamine, making it difficult to experience pleasure from natural sources, such as eating, socializing, or exercising. This reliance on a drug for dopamine rewards is one of the key drivers in the cycle of addiction.
Tolerance: The Brain’s Adaptation to Substance Use
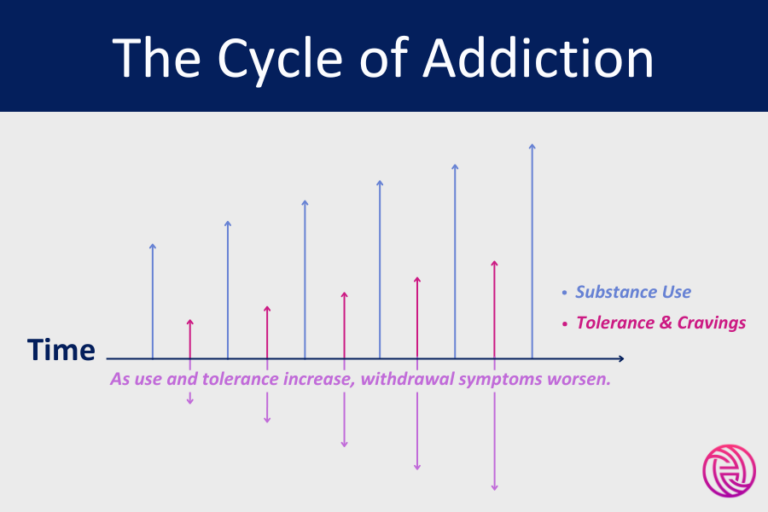
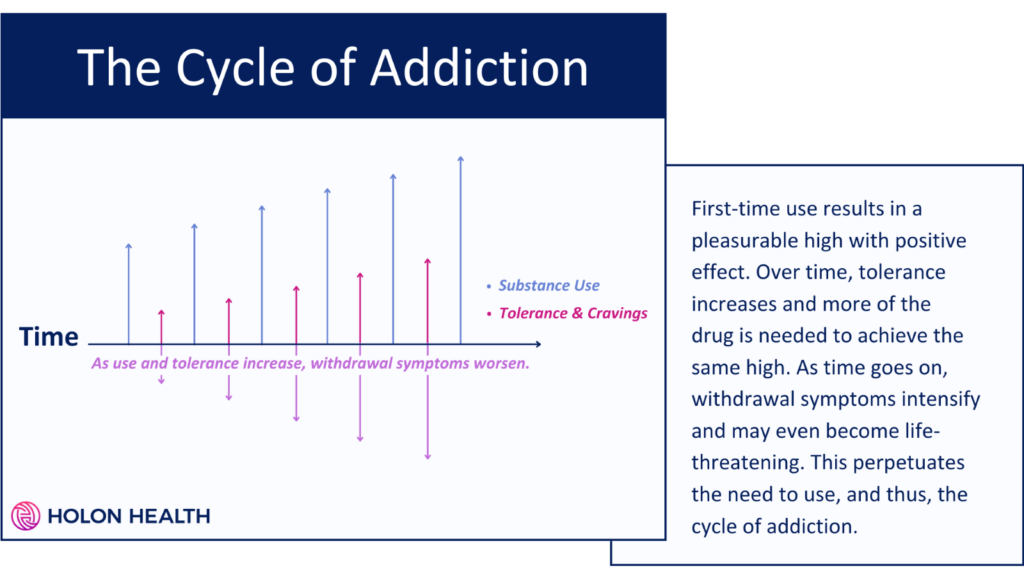
As drug use continues, something known as tolerance develops. Tolerance occurs when the brain becomes accustomed to the increased dopamine levels caused by drug use. To achieve the same euphoric feeling, a person needs to take larger doses of the drug. Essentially, the brain “raises the bar” on how much of the substance is required to trigger a dopamine response.
This means that over time, users need to consume higher amounts of the drug to feel its effects, further reinforcing the cycle of addiction. The more the brain adapts, the more drugs are needed, leading to even more profound changes in brain chemistry.
A Visual Look at the Cycle of Addiction
Withdrawal: The Body’s Response to Absence
When a person tries to stop using the substance, withdrawal symptoms often follow. These symptoms vary depending on the drug but can include anxiety, irritability, nausea, depression, and physical pain. Withdrawal occurs because the brain, after becoming reliant on the drug for dopamine production, struggles to function normally without it.
During addiction, the brain’s natural production of dopamine becomes suppressed, and without the drug, dopamine levels plummet, leading to intense cravings and withdrawal symptoms. This state is both physically and emotionally painful, which often drives individuals back to substance use to relieve their discomfort.
The Alpha Cells and GABA System’s Role in Addiction
Beyond dopamine, other elements of brain chemistry contribute to the cycle of addiction. Alpha cells located in the pancreas produce glucagon, a hormone that helps regulate blood sugar. While these cells are primarily associated with metabolic processes, some research suggests they might have a role in how the brain regulates energy and reward pathways during addiction.
Additionally, the Gamma-Aminobutyric Acid (GABA) system is crucial in understanding addiction, especially in the context of substances like alcohol or benzodiazepines. GABA is the brain’s primary inhibitory neurotransmitter, which helps to calm neural activity. Many addictive substances, especially depressants, enhance GABA activity, leading to relaxation and sedation. However, prolonged use can desensitize the brain’s GABA receptors, making it harder for the brain to regulate anxiety and stress without the substance. This leads to further dependency.
How Addiction Alters Brain Chemistry
Repeated substance use doesn’t just affect neurotransmitters temporarily; it alters the brain’s overall chemistry and structure. These changes are particularly noticeable in areas involved in decision-making, impulse control, and judgment, such as the prefrontal cortex.
Over time, addiction impairs the brain’s ability to regulate its own neurotransmitters, including dopamine and GABA. This creates a constant state of imbalance, where the brain’s natural systems can no longer function properly without the drug. As a result, people struggling with addiction cycles often find it difficult to make rational decisions or resist cravings.
How to Break the Cycle of Addiction
Breaking the cycle of addiction requires more than willpower. Because addiction is rooted in profound brain chemistry changes, treatment must address these underlying issues. This often involves:
- Detoxification: Helping the body cleanse itself of the substance.
- Medication: Some medications can help restore balance to neurotransmitter systems like dopamine and GABA, reducing cravings and withdrawal symptoms.
- Therapy: Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), and other forms of counseling can help rewire the brain’s response to cravings and stress.
- Support Systems: Addiction recovery is greatly supported by peer groups, counseling, and family therapy to maintain long-term sobriety.
The cycle of addiction is a powerful and destructive process fueled by changes in brain chemistry, tolerance, withdrawal, and neurotransmitter regulation (or disregulation). While dopamine is the star player in the brain’s reward system, other components like alpha cells and the GABA system also contribute to the persistence of addiction. Understanding the biological underpinnings of addiction can pave the way for more effective treatments and help those struggling break free from its grasp.
Breaking the cycle of addiction is challenging, but with the right support and treatment, it is possible to reclaim control over one’s life. By addressing the brain’s complex chemistry and the emotional aspects of addiction, individuals can find a path to recovery.
Get Help Today
Addiction doesn’t have to be forever. If you or someone you love is struggling with substance use, Holon Health can help. We use the power of positive motivation combined with cash rewards to keep you on the road to recovery. We offer telehealth services, medication management (including prescriptions like Suboxone), recovery coaching, and so much more. Our services are covered by Medicaid/Medicare and come at no cost. To enroll today, click here. To learn more, call (877) 465-6650.
References:
- National Institute on Drug Abuse (NIDA). “Drugs, Brains, and Behavior: The Science of Addiction.” NIDA, 2020.
- Volkow, Nora D., et al. “Neurobiologic Advances from the Brain Disease Model of Addiction.” New England Journal of Medicine, vol. 374, no. 4, 2016, pp. 363-371.
- Koob, George F., and Michel Le Moal. “Addiction and the Brain Antireward System.” Annual Review of Psychology, vol. 59, no. 1, 2008, pp. 29-53.
- Riegel, Arthur C., and Paul E. Kalivas. “The GABA System in the Central Nucleus of the Amygdala Contributes to Opioid Dependence.” Neuropsychopharmacology, vol. 30, no. 2, 2005, pp. 537-544.
- Sapolsky, Robert M. “The Physiology and Pathophysiology of Glucocorticoids in the Nervous System.” Progress in Neurobiology, vol. 9, no. 1, 2000, pp. 45-47.